How Advil and Tylenol Supercharge Antibiotic Resistance
Photo by Wirestock
Antimicrobial resistance (AMR), the development of resistance by germs to the medicines meant to kill them, is one of the most concerning looming health crises in the world right now. While the most obvious and direct reason for this issue is the overuse of antibiotics, a sneaky, new cause has recently been discovered through new research. A study by researchers at the University of South Australia (UniSA) has revealed that the use of non-antibiotic medicines (NAMs), such as common painkillers, can significantly accelerate the rate at which germs adapt to these medicines. Published August 25, 2025, in Nature Microbiology, this groundbreaking research broadens the scope of what doctors and scientists should focus on in the realm of combating AMR across the globe.
The team at UniSA designed an experiment to test the effects of some of the most popular NAMs, such as acetaminophen (found in Tylenol) and ibuprofen (found in Advil), when used concurrently with antibiotics. Specifically, they investigated the level of adaptation in E. coli bacteria against one of its most common antibiotics, ciprofloxacin. They set up multiple groups to test this. The first was a control group of E. coli treated only with ciprofloxacin. The others were groups of E. Coli, which were treated with ciprofloxacin and either one or two of nine different non-antibiotic medicines. They looked at these different groups for rates of adaptation and resistance. In simple terms, the independent variable was the presence of non-antibiotic medicines, and the dependent variable was the level of antibiotic resistance in the E. Coli. To ensure the accuracy of the results, the researchers conducted the tests in both humans and in more controlled laboratory cultures.
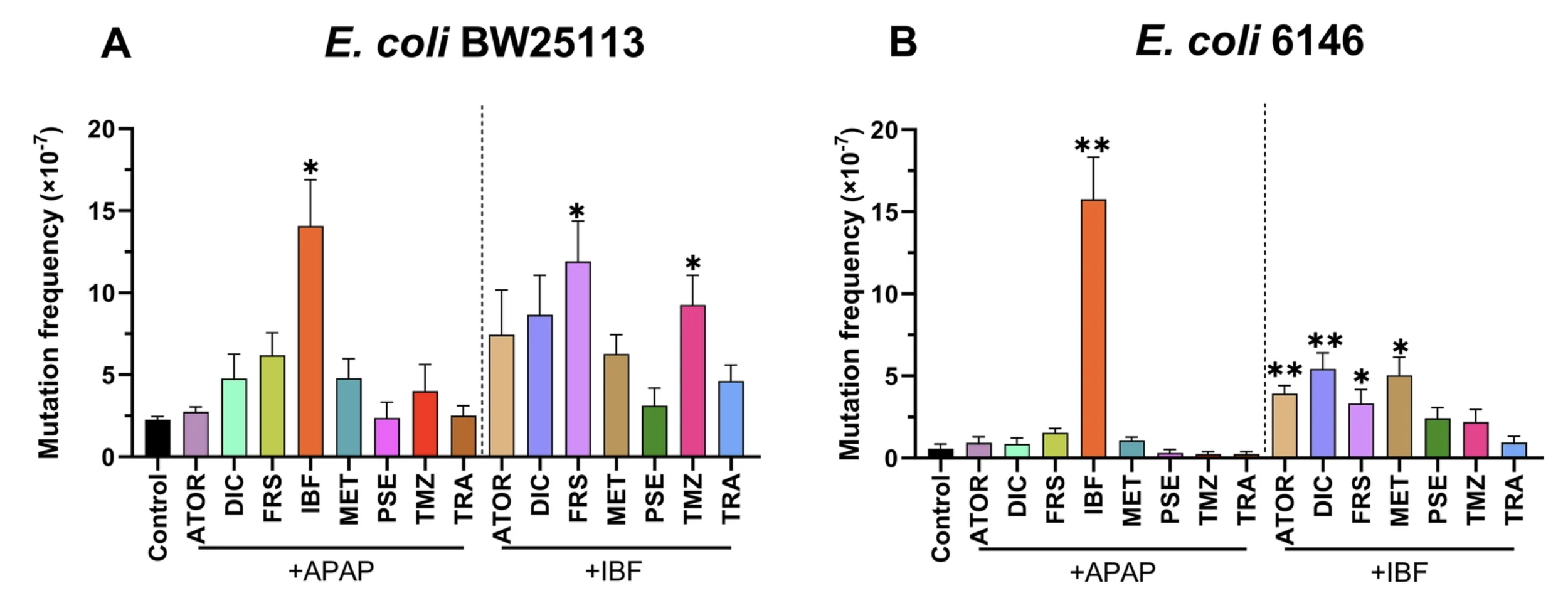
The results the team found were massive. Not only did the E. Coli that was exposed to non-antibiotic medicines develop antibiotic resistance faster than the E. Coli that was only exposed to ciprofloxacin, but the combination of ibuprofen and acetaminophen, two of the most common NAMs, caused the fastest acceleration of AMR in the E. Coli. In fact, the E. coli exposed to both acetaminophen and ibuprofen, in combination with ciprofloxacin, developed resistance to a variety of antibiotics upon further testing. The genetic testing revealed that non-antibiotic medicines led to higher mutation rates, resulting in the development of more evolved strains that confer resistance to antibiotics. In practical terms, this means that the Tylenol or Advil taken to help with the side effects of sickness may actually be making it harder to treat the sickness itself.
Above, it is shown that bacteria exposed to both painkillers and antibiotics showed significantly higher mutation frequencies, and thus more resistant colonies than those exposed to antibiotics alone.
The implications of these findings are extremely far-reaching. AMR was predicted to have killed 4.9 million people in 2019. The global population is aging, and with age comes an increased risk of illnesses and chronic illnesses that require antibiotics and non-antibiotic medicines. This means that the issue is only expected to worsen over time. As stated, the use of non-antibiotic medicines is rising sharply, particularly in elderly care and long-term health management settings associated with this aging global population, where patients often rely on painkillers and anti-inflammatory drugs alongside other treatments. If these medications are enhancing AMR, they create a hidden danger of ordinary symptom-relief drugs amplifying one of medicine’s greatest threats. This study emphasizes the need to expand research on AMR beyond the antibiotics themselves and examine the role of all contributing factors. Of course, it is not feasible to stop using NAMs completely, but the study does pose questions for physicians on how to possibly moderate their usage. By shedding light on a previously understudied aspect of AMR, the research can help elucidate the impact of NAMs and pave the way for discovering new strategies to mitigate resistance and preserve the effectiveness of antibiotics, which are becoming increasingly crucial.